Some cardiac arrhythmias are exciting and fun for the prehospital provider. Ventricular fibrillation has, essentially, only one proven therapy, but needs a well-choreographed team to deliver it. Paroxysmal supraventricular tachycardia,
on the other hand, has a far less dire prognosis, but the treatment is
generally safe and dramatic - very satisfying for both the patient and
provider!
Unlike
VF or PSVT, however, atrial fibrillation isn’t a fun rhythm to deal
with, either in-hospital or prehospital, and there are many ways to screw up. Even
the new edition of Nancy Caroline's Emergency Care in the Streets has little to say about management of atrial fibrillation, only mentioning that
They are likely correct about the "rare" part - one study of atrial fibrillation treated by EMS backs this up - you just aren't likely to have a patient with atrial fibrillation that needs cardioversion or emergent diltiazem. On the other hand, atrial fibrillation is really common in EMS, and we should know a bit more about this. There are lots of recent articles and old insights about AF - how about we start with 4 things?
 |
|
"Prehospital treatment of atrial fibrillation is rare because of the risks involved."However, they don't describe those risks, or how to avoid them!
They are likely correct about the "rare" part - one study of atrial fibrillation treated by EMS backs this up - you just aren't likely to have a patient with atrial fibrillation that needs cardioversion or emergent diltiazem. On the other hand, atrial fibrillation is really common in EMS, and we should know a bit more about this. There are lots of recent articles and old insights about AF - how about we start with 4 things?
1. AF is often a symptom, not the disease
Some
rhythms require treatment, regardless of the history or exam. In other
words, sometimes we "treat the monitor." AF is not like this.
Example: A medic recently brought us an older female with palpitations. Evidently this had started about 3 hours prior, and was just getting worse. She had been taking all her "heart pills," but had had some vomiting and diarrhea for the past day and a half. Her HR was 180, and she was somewhat hypotensive at 95/60. Her sat and RR were basically normal.
Example: A medic recently brought us an older female with palpitations. Evidently this had started about 3 hours prior, and was just getting worse. She had been taking all her "heart pills," but had had some vomiting and diarrhea for the past day and a half. Her HR was 180, and she was somewhat hypotensive at 95/60. Her sat and RR were basically normal.
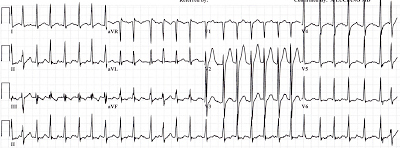
A 12-lead was obtained:
ST-segment changes, rapid AF and hypotension - should the patient receive diliazem, metoprolol, or even cardiovert? These can the right answers for many rhythms with & without hypotension (e.g. VT, PSVT), but AF can be different.
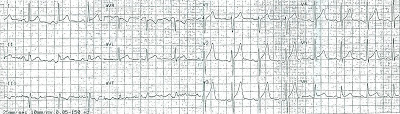
The medic decided, based on the recent history of volume losses, that a fluid bolus should be tried. After 300 ml of NS he saw a change in heart rate, and recorded ECG #2:
The blood pressure settled out at 120s/70s, and the rest of transport was uneventful. She ended up getting some diltiazem in the ED, but it looked more like dehydration that caused her tachycardia, as well as impaired absorption of her medications.
This is very common - AF is often provoked or worsened by non-cardiac problems. A drinking binge can do it, and so can hyperthyroidism. A low magnesium, in some cases, may be responsible. Both a large pulmonary embolus (because of the right atrial strain), and an MI, may kick off AF. And as for alcohol...
2. Alcohol (too much or too little) and AF.
He was weak, had vomited at least 10 times that day, and couldn't stop shaking. This 40 y.o. man had stopped drinking 2 days ago, and had not done well since. The palpitations were the final straw, pushing him to come to the ED.
 |
|
"Excuse me, did something crawl down your throat and die" "It didn't die!" |
His labs confirmed that he has dehydrated, with low levels of magnesium and potassium. His alcohol history, both the excess, and the abrupt cessation, also likely contributed to provoking a new-onset atrial fibrillation.
He clearly didn't need cardioversion, but it also seemed premature to use diltiazem or metoprolol first. He received a liter of saline, some magnesium and potassium, as well as Valium for the withdrawal. This went a long way towards improving his heart rate, and he only needed a small dose of metoprolol after all that.
So, while he had atrial fibrillation, he had other medical issues (like the withdrawal) that were more important. This is actually pretty common - about 75% of patients who come to the emergency department who have AF on their ECG actually have a different primary diagnosis - the top three diagnoses are CHF, pneumonia, and chest pain.
 |
| Patients with AF and an Alternative Primary Diagnosis in the ED |
3. This is especially true for sepsis and AF.
I recently saw a patient brought in from a nursing home with AF at 170-180 bpm, as well as hypotension. Sorta looked like this:
 |
| LITFL |
This case was not unusual - it turns out there is a HUGE relationship between sepsis and AF. Some surprising facts:
- New-onset AF happens in > 6% of severe sepsis cases (or even 46%!)
- 14% of new-onset AF cases in the hospital occur during severe sepsis
- Mortality of patients w/ severe sepsis and new-onset AF is > 50%
 |
| AF & sepsis = bad news bears. |
It isn't clear how AF should be treated in severe sepsis, besides treating the source of infection and supportive care. The use of rate-controlling medications (diltiazem and metoprolol) may "mask" the signs of sepsis, complicating the use of fluid boluses or pressors. Cardioversion with drugs or electricity pose their own hazards.
So, if your nursing home patient has new AF, think: Could this be sepsis?
To be continued!
So far these patients I've discussed haven't been terribly unstable. In my last example (to be posted soon!) I'll discuss a truly critical patient with paroxysmal AF, where cardioversion was not performed. I've already shown the ECG on the Mill Hill Ave Command Facebook page, but I'll share more elements, and how they relate to management.